
Atrial fibrillation (AF), a frequently encountered cardiac arrhythmia, presents notable diagnostic challenges to healthcare practitioners. Despite substantial advancements in cardiac care and technology, the early detection of AF continues to be an elusive task with important consequences. As I discussed in my last post, advances in artificial intelligence (AI) may be creating new avenues to assist us with this endeavor. In this sophisticated AI landscape, another pioneering study was recently published in Nature Digital Medicine. This research presents the feasibility of predicting future AF from single-lead ECG recordings captured remotely. Harnessing the capabilities of digital health solutions and the cutting-edge advancements in AI, we are continuing to revolutionize the approach towards AF screening and diagnosis.
Why is it Important?
AF increases your risk of stroke by 5-fold (which can be managed with appropriate anticoagulation) and up to 35% of people with AF remain undiagnosed, in-part because we lack proven, cost-effective measures for AF screening and it is not recommended by the USPSTF. Identification of patients at increased risk of AF can enable a more targeted screening strategy so that we can focus our AF monitoring efforts on those individuals at the highest risk with the most to gain.
Nature Digital Medicine Study
In this paper, the authors Gadaleta et al. present the development of a deep learning model to estimate the risk of near-term AF based on AF-free single-lead ECG recordings of various lengths. The authors used 459,889 patch-based ambulatory ECG recordings (iRhythm Zio® XT) of up to 14 days from patients who underwent continuous monitoring for suspected AF. They extracted ECG morphology features, demographic metrics, and heart rate variability (HRV) features from the recordings and trained a deep neural network to predict the probability of AF occurrence in the next 14 days. They evaluated model performance using the area under the receiver operating curve (AUC) metric, comparing models that looked at various combinations of demographic data, HRV data, and deep learning (DL) features that were automatically extracted by the model during training from the ECG data.
The primary findings were as follows:
- The model utilizing only demographic data had an AUC of 0.67 (CI: 0.66-0.68), the model with demographic and HRV data had an AUC of 0.74 (CI: 0.72-0.75) and the model utilizing all features (demographics, HRV and DL features) had an impressive AUC score of 0.80 (0.79-0.81).
- The model utilizing only DL generated features had a minimal difference to the all features model, with an AUC of 0.79 (difference of <0.01 [CI: 0.00-0.01; p=0.02]).
- Model performance varied by age, monitoring length, and AF burden. Notably, the model performed better for younger individuals, longer ECG windows, and higher AF burden.
This study demonstrates the feasibility of predicting future AF episodes using deep learning and a single-lead ECG obtained from a chest patch. DL analysis of the ECG morphology significantly improved prediction accuracy compared to traditional features like demographics and heart rate variability. Longer monitoring periods further enhanced prediction, suggesting the presence of dynamic AF indicators not always captured in short recordings. Similar to other recent work (previously reviewed on this blog), this novel approach holds promise for identifying individuals who would benefit most from screening with extended ECG monitoring. Overall, the findings pave the way for a novel digital strategy of AF risk assessment and personalized monitoring, potentially leading to improved clinical outcomes (see the case study below, provided by authors of the study). Further validation in prospective studies and integration with additional clinical data are necessary before widespread clinical implementation.
Potential Use Case
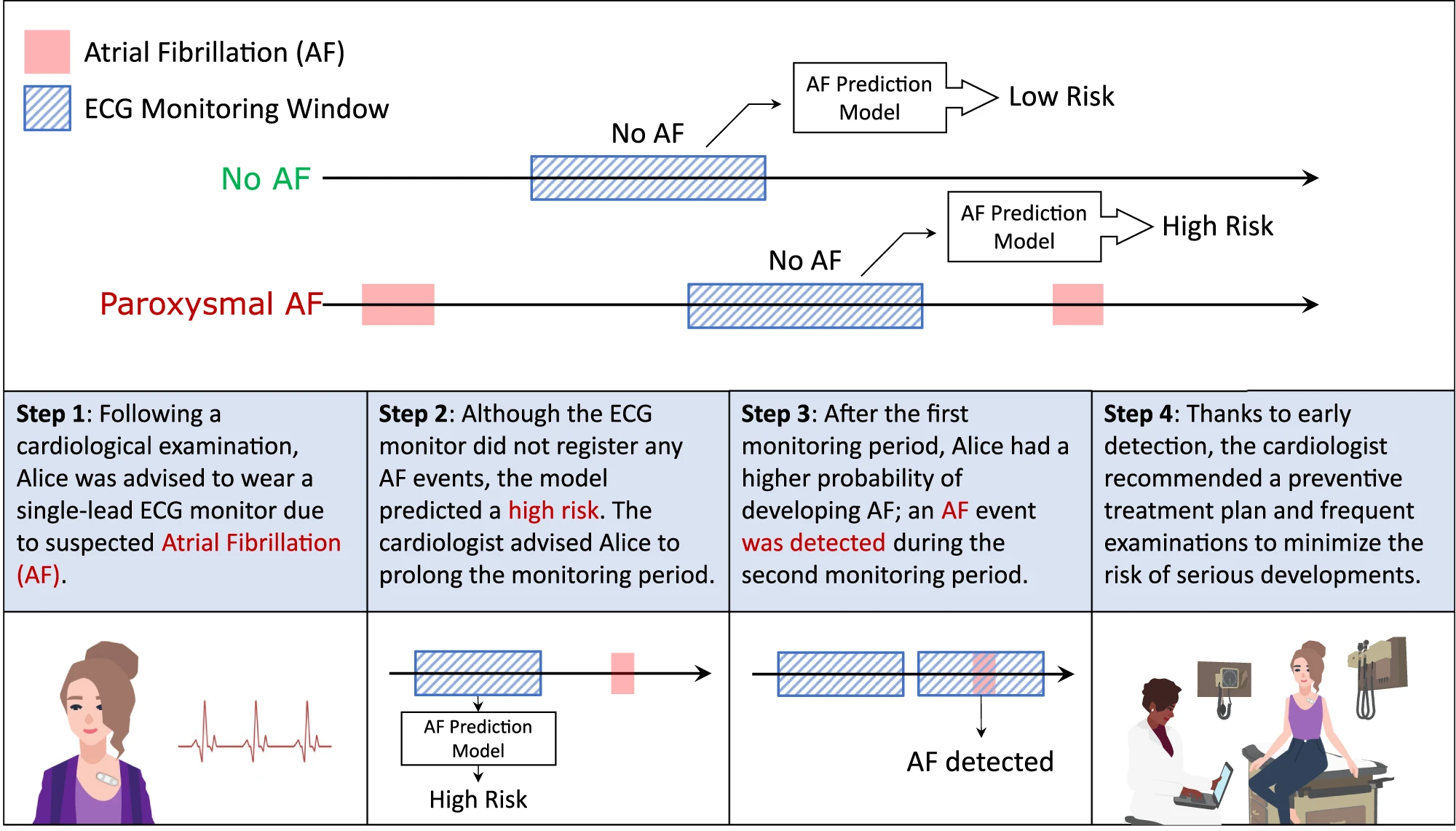
Source: NPJ Digital Medicine 6, 229 (2023). DOI: 10.1038/s41746-023-00966-w
Please subscribe to our Newsletter for email notifications containing new posts as soon as they are published:
