Google’s 2025 research paper “The Anatomy of a Personal Health Agent” describes a prototype multi-agent AI framework designed to turn raw health data into personalized, evidence-based guidance. In this post we will review the paper and the urgent need for this technology and the new type of AI Service that it represents.
The Urgent Need for a Health Revolution
Walk into any clinic today and you’ll see the same well-described paradox playing out: we live in an age of unprecedented medical knowledge and technology, yet most of our healthcare still revolves around reacting to disease. We call it a healthcare system, but in practice it’s a sick-care system—one that waits for illness before engaging.
The consequences are everywhere: Physicians are burning out under crushing time and administrative loads; health systems face record costs from chronic conditions that could have been mitigated with earlier action; and patients, surrounded by wearable sensors, health apps, and lab portals, sit atop mountains of personal data that largely go unused.
The great opportunity of our time is to shift from repairing health to maintaining it. That shift—toward proactive, data-driven prevention—requires more than good intentions or new gadgets. It requires a system that can understand an individual’s unique health signals, contextualize them against medical knowledge, and translate them into daily action.
That is exactly what Google’s Personal Health Agent (PHA) research framework sets out to explore.
Rather than a single “chatbot,” the PHA represents a research architecture for intelligent, multi-agent collaboration that puts the individual and their wellness journey at the center. Built by researchers at Google and DeepMind, the PHA is designed to interpret multimodal health data—from wearables to lab results—and deliver personalized, evidence-based coaching that empowers people to take control of their health.
It’s not currently a product, and it’s not available to consumers at this time, but conceptually, it points to something profound: a future in which AI isn’t simply a tool to answer health questions—it’s a service that is helping you understand your own biology in real time and make changes needed to stay healthy.
The Technological Leap: Why Now?
For decades, the promise of “personalized healthcare” has outpaced the technology to deliver it. We had electronic health records (EHR), wearable devices, and scattered apps—but they spoke different languages. True personalization requires an intelligence capable of interpreting all of these streams together.
The AI Moment
The breakthrough comes from a now familiar source: multimodal large language models (LLMs). Over the past few years, models like Gemini, GPT, and Claude have learned to process not just text but images, code, and even structured data. This ability to understand and reason across modalities has quietly unlocked a new class of health tools.
The PHA builds directly on that progress. It treats AI not as a black box that spits out answers, but as an orchestrated service that reasons about your health the way a multidisciplinary care team might. The system’s architecture—rooted in multimodal reasoning and multi-agent collaboration—is what allows it to move beyond symptom checkers and toward a genuine health advisor.
Why Multimodal Matters
Multimodal data is the missing ingredient in digital health. Your wearable produces continuous time-series signals—heart rate, sleep patterns, step counts, heart-rate variability. Your health record portal adds labs, imaging, and past medical diagnoses. Your own words (“I’ve been more tired lately”) introduce context no device can capture.
Each of these alone is useful, but together, they form a more comprehensive picture of your physiology.
Yet until recently, no AI system could reliably interpret that mixture. Previous models could answer general medical questions or were built to analyze specific data types, but not both at once. The PHA is an advanced framework designed to reason across modalities—to read your wearable data, compare it to clinical norms, understand its significance in the broader picture of your past health, and weave it into natural conversation and advice.
AI as a Service, Not just a Tool
Another key shift is conceptual. In healthcare, the technology itself is only part of the story. What often matters more is how it’s used. The PHA reframes AI from being a tool that generates outputs to being the engine of a personalized health service—one that can listen, analyze, contextualize, and coach.
Instead of AI that answers your questions, think AI that understands your health narrative and helps you act on it. That evolution—from model to service—marks the difference between passive information delivery and active health empowerment.
The Anatomy of a Digital Coach
So what exactly lives inside Google’s Personal Health Agent?
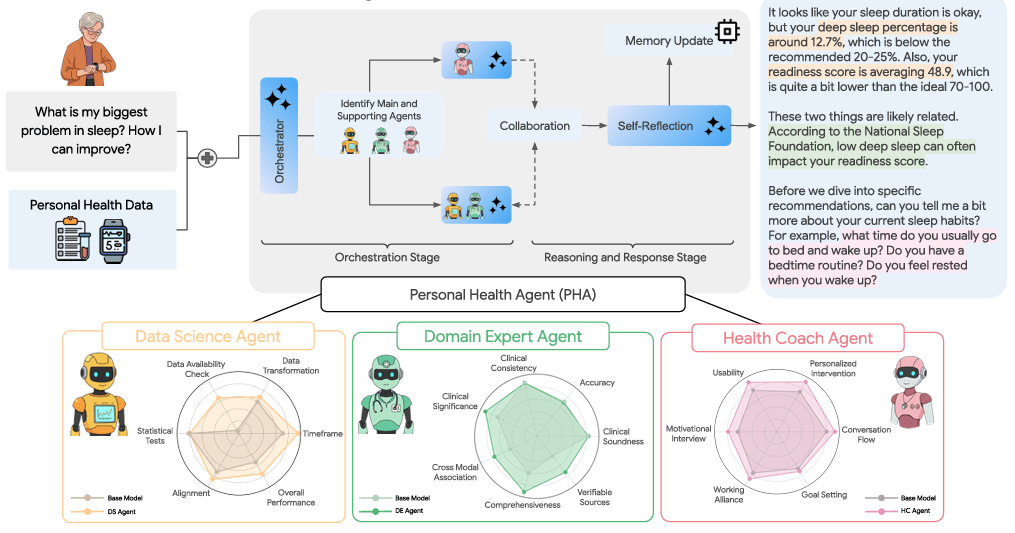
At its core, the PHA is a multi-agent ecosystem, each component representing a distinct area of expertise, coordinated by an intelligent Orchestrator (similar to Microsoft’s MAI-DxO). The design mirrors how real healthcare teams operate—different specialists collaborating under a shared mission to support the patient.
1. The Data Science Agent (DS Agent)

Think of the DS Agent as your personal data scientist. Its job is to analyze complex time-series data—your daily steps, sleep duration, heart-rate trends—and translate those signals into meaningful insights.
If you ask, “Am I getting fitter?” the DS Agent doesn’t just check your step count; it compares recent activity trends, adjusts for missing data, and benchmarks you against population norms. It can generate a full analysis plan—choosing appropriate statistical tests, cleaning the data, and even writing executable code to produce the results.
In testing, Google’s researchers found that this structured multi-stage approach (plan → code → validate) dramatically improved both accuracy and robustness compared to standard LLM outputs. In essence, the DS Agent is what makes your raw data actionable.
2. The Domain Expert Agent (DE Agent)
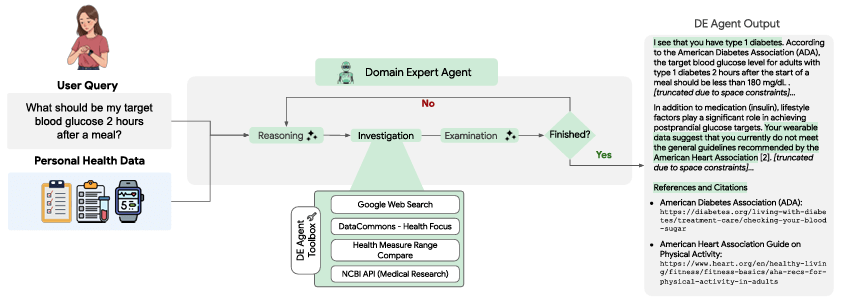
Once the data are analyzed, interpretation matters. The DE Agent acts as the system’s medical brain, grounding insights in evidence-based health knowledge.
If the DS Agent identifies elevated resting heart rate variability, the DE Agent explains what that means in context—drawing on literature from medical databases like NCBI and population-level statistics from Data Commons. It can use data from across modalities (wearables + labs + notes), perform differential diagnosis, and tailor outputs to your individual health profile.
Evaluations showed the DE Agent outperforming base models on expert-level medical exams, contextual accuracy, and trustworthiness when generating multimodal health summaries. In short, it bridges personal data with medical science—something traditional chatbots have struggled to do well.
3. The Health Coach Agent (HC Agent)
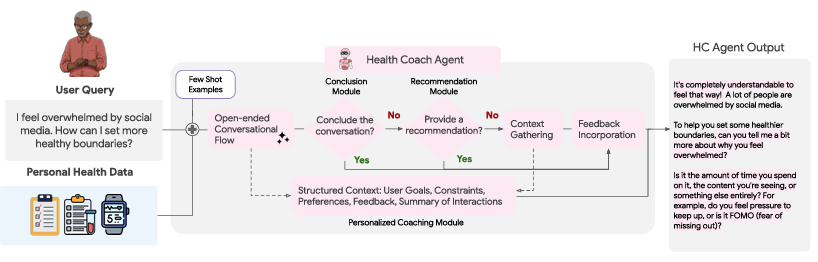
Data and expertise are only part of the equation; active behavior change is the ultimate goal. The HC Agent translates insight into action through goal-oriented dialogue. Borrowing from techniques like motivational interviewing, it engages users in multi-turn conversations to set achievable goals, identify barriers, and track progress. For example:
“Your average sleep dropped by 45 minutes last week. What do you think contributed to that?”
“Would you like to experiment with a consistent bedtime this week and review the results on Friday?”
It is also not a static coaching app that delivers one-off advice, the HC Agent adapts dynamically—its recommendations evolve as your data and circumstances change.
4. The Orchestrator: A Hidden Conductor
Overseeing this team is the Orchestrator, a higher-level agent responsible for routing queries, coordinating sub-agents, and synthesizing their outputs into coherent responses.
When you ask a compound question—“Why did my sleep score drop, and what should I do about it?”—the Orchestrator decides that the DS Agent should first analyze the data, then directs the DE Agent to interpret the findings, and finally prompts the HC Agent to bring you insights and help guide behavior change.
The result feels like a single, seamless conversation—yet behind the scenes, multiple AI experts have collaborated, debated, and refined the answer. This architecture is what makes the PHA a system, not just a model. It integrates data science, medical reasoning, and behavioral psychology into one coordinated digital service.
The Impact: From Reactive Care to Preventative Wellness
Proactive Detection and Early Intervention
Imagine an agent that notices subtle shifts in your resting heart rate, stress levels, or sleep efficiency—days to weeks before you would. By continuously analyzing wearable trends and contextualizing them with lab or lifestyle data, the PHA could flag potential issues early and prompt timely action or prompt you to alert your medical team.
This is the essence of primary prevention: catching deviations before they escalate into disease. Over time, as more data accumulate, the system could also support secondary prevention, helping those with chronic conditions maintain stability through personalized insights.
Empowerment Through Understanding
For most people, health data are cryptic. The PHA’s conversational layer changes that. Instead of a dashboard of numbers, users can ask for an interpretation: “Why is my HRV trending lower?” or “How do my sleep patterns affect my glucose?” and receive an interpretable, evidence-based explanation.
This interpretability isn’t just convenience; it’s empowerment. When people understand their data, they are far more likely to act on it. The PHA turns passive metrics into an feedback loop that supports self-efficacy.
Bridging the AI-Human Divide
Crucially, Google’s researchers emphasize that the PHA is not meant to replace clinicians. Rather, it complements them by translating continuous personal data into structured, interpretable summaries. Picture visiting your doctor with a month-long “digital health snapshot” automatically generated by your PHA—highlighting patterns, correlations, and progress.
Instead of starting from scratch, your physician starts from insight. The result: more productive visits, better shared decision-making, and reduced clinician burden.
A Blueprint for Responsible AI in Health
The paper also underscores a vital principle: safety and accountability must be built into the architecture. Each agent is evaluated against rigorous benchmarks—over 7,000 expert annotations and 1,100 hours of human evaluation across 10 tasks.
This evaluation framework is just as important as the technology itself. It provides a roadmap for auditable, modular AI systems in healthcare—ones that can be validated, refined, and regulated more effectively than monolithic models.

The Road Ahead: Health as a Service
The PHA marks a conceptual turning point. For years, digital health has focused on data collection—the next smartwatch metric, the next health app. The PHA suggests the next frontier is data interpretation as a service. Picture a world where:
- Your wearable syncs with a personal health agent that learns your baseline and adapts daily coaching accordingly.
- Your medical record isn’t a static file but a living model of your health trajectory that directs active guidance and recommendations.
- Instead of annual checkups, you have continuous dialogue—AI-mediated when routine, human-led when complex.
In this future, the doctor and health system don’t disappear, they gain a teammate and assistant who works 24/7, tracking, explaining, and motivating between visits.
Challenges and Cautions
Of course, immense hurdles remain. Privacy and data consent must be handled with uncompromising rigor. Models must be validated and bias-audited, especially when guiding behavior. And perhaps most importantly, society must decide how such systems integrate with clinical care—who’s accountable when an algorithm misses a warning sign, and how do we ensure equitable access.
But the general direction and path forward is clear: the fusion of multimodal AI and personal health data should empower patients, assist clinical teams, and streamline care, leading to a healthier population and less burdened healthcare infrastructure.
The Future: Where AI Can Take Us
The PHA represents far more than an impressive AI tool. It embodies a vision of healthcare’s future—one where technology empowers individuals rather than replacing human judgment, where prevention is prioritized over intervention, and where personalized health guidance is accessible to everyone, not just those who can afford personal health coaches and concierge medicine.
We stand at a remarkable inflection point. We now have both the data and the intelligence to understand individual health patterns with unprecedented granularity. The PHA demonstrates that we can weave these strands together—multimodal data, advanced AI, medical knowledge, and behavioral science—into a coherent service that makes preventative healthcare not just theoretically possible but practically achievable.
The implications ripple outward: fewer preventable hospitalizations, earlier intervention for chronic conditions, reduced healthcare costs, and individuals empowered with the knowledge and support to take control of their wellness journey. The PHA shifts the burden from overwhelmed healthcare systems to proactive, informed individuals supported by intelligent digital agents.
But perhaps the most exciting aspect is what this research unlocks for the future. The PHA is a proof of concept that establishes feasibility and points the way forward. As these technologies mature and are responsibly deployed, we move closer to a world where the thousands of health data points you generate daily aren’t just passively collected but actively transformed into personalized wisdom that helps you live healthier, longer, and better.
Follow us on Substack:
To ensure timely access to posts and future updates, be sure to subscribe to This week in Cardiovascular AI – an email newsletter for followers and subscribers that summarizes recent research in Cardiovascular AI.
